Hypercholesterolaemia is also known as dyslipidaemia, which refers to high levels of cholesterol in the blood. There are various causes and contributing factors that can lead to hypercholesterolaemia.
What is hypercholestrolaemia?
Hypercholesterolaemia is the condition of having abnormal levels of cholesterol in the blood. The body obtains cholesterol from the foods we eat and from the cholesterol synthesis of the cells. The liver is the main site where cholesterol homeostasis (balance) is maintained. Lipoproteins are complex particles responsible for the transport of fats including cholesterol and triglycerides in the body.
Lipoproteins
Lipoproteins are particles of fats and proteins consisting of a cholesterol or triglyceride core, surrounded by free cholesterols, phospholipids and apolipoproteins. Several types of lipoproteins are found in our body:
- High-density lipoprotein (HDL) – HDLs have high proportions of proteins to lipid, their main function is to transport cholesterol from the bloodstream to the liver. HDLs also have anti-inflammatory properties due to their ability to reduce the size of atherosclerotic plaques.
- Intermediate-density lipoprotein (IDL) – IDLs are derived from very low-density lipoproteins. IDLs are also pro-atherogenic, which promotes the formation of atherosclerosis plaques.
- Low-density lipoprotein (LDL) – LDLs are derived from VLDL and IDL particles. LDLs carry the majority of cholesterol that is found in the blood.
- Very low-density lipoprotein (VLDL) – Similar to LDLs, VLDLs transport cholesterols and triglycerides from the liver to the blood.
- Chylomicrons – Chylomicrons are large triglyceride-rich particles made by the intestine. These particles carry dietary lipids from our food.
The term high cholesterol is often associated with high levels of Non-HDL lipoproteins (Mainly LDL). High levels of LDL which we know is responsible for deposition of cholesterol into blood vessel walls will eventually lead to a higher level of atherosclerotic plaque formation. Rupture of these plaques or blockage of blood vessels by these plaques lead to cardiovascular and vascular diseases such as heart attack.
What are the signs of hypercholestrolaemia?
Hypercholesterolaemia in itself does not show symptoms. Symptoms occur when it’s too late, when cholesterol plaque blocks or ruptures causing heart attack, stroke and peripheral vascular disease (poor circulation in the legs). With very high levels of cholesterol (often seen in genetic/ familial hypercholesterolaemia) the following might be seen:
- Xanthoma – Xanthomas are deposits of fat underneath the skin and soft tissues such as tendons. Xanthomas are caused by the breakdown of lipoproteins.
- Xanthelasma palpebrarum – Xanthelasma palpebrarum is characterised by soft or semi-solid yellow papules consisting of cholesterol. These papules are often found near the inner corners of the eyes, along the upper and lower eyelids. Xanthelasma palpebrarum is also considered a form of xanthoma. The papules are formed from the accumulation of lipids in macrophages.
Arcus cornealis – Arcus cornealis, sometimes known as arcus senilis, is the appearance of gray or white rings of lipid around the outer cornea. Although common in elderly people, arcus cornealis in younger people are typically associated with hypercholesterolemia.
What causes hypercholestrolaemia?
Hypercholesterolaemia or dyslipidaemia can be familial (genetically inherited) or acquired (develops over time).
Familial hypercholesterolaemia
Familial hypercholesterolaemia is inherited genetically, these are typically caused by genetic mutations leading to the impaired ability of the liver to take up circulating LDL-cholesterol (LDL-C) in the blood. The reduction in LDL removal by the liver results in very high LDL levels. Common examples of inherited familial hypercholesterolaemia include:
- Mutation of the LDL receptor – Loss-of-function mutations to the gene that codes for the LDL receptor causes a reduction in the activity of the receptors to take up excess LDL-cholesterol from the blood.
- Mutation of the gene coding the apolipoprotein – Mutations to this gene can cause the shape of the apolipoprotein to change, hence reducing the ability of the protein to attach to the LDL receptor in the liver.
- Increased clearance of the LDL receptors – A gain-of-function mutation of an enzyme known as proprotein convertase subtilisin/kexin type 9 (PCSK9) causes an increase in the removal of LDL receptors on the liver cells surfaces. Ironically this mechanism has been harnessed in cholesterol treatment.
Familial hypercholesterolaemia must be screend and treated early. Much can be done with early and personalised treatment. Patients with familial hypercholesterolaemia are pre-disposed to heart attack and strokes in their 40s or earlier. A family history of early heart attack or stroke may be indicative.
Acquired hypercholesterolaemia
Acquired hypercholesterolaemia is typically secondary to causes such as:
Who is at risk of hypercholesterolaemia?
Common risk factors of hypercholesterolaemia include:
- Age – The risk of dyslipidaemia is typically higher in men 45 years and older, or in women 55 years and older.
- Family history – Having a family member with premature atherosclerotic heart disease (younger than 55 years in men, and younger than 65 years in women) also increases your risk of Hypercholesterolaemia.
- Diabetes – Diabetes and hypercholesterolaemia often co-exist and both contribute to an increased risk of cardiovascular diseases.
- Hypertension – Similarly, hypertension and hypercholesterolaemia are also associated with each other. Hypertension can increase the risk of atherosclerosis leading to an increased risk of cardiovascular diseases.
How is hypercholesterolaemia diagnosed?
Typically, your healthcare provider will recommend you to get a lipid panel, sometimes also called a lipid profile. This test shows you the levels of your:
- Total cholesterol – Total cholesterol measures your overall cholesterol, including LDL-C, HDL-C, and VLDL-C.
- LDL-C – LDL-C in the blood is also known as the “bad cholesterol”. LDL-C can cause cholesterol deposition in blood vessel walls and increase atherosclerotic plaque.
- HDL-C – HDL-C in the blood is known as “good cholesterol”, which helps transport cholesterol back to the liver.
- Triglycerides – Triglycerides are fats from our diet, high levels of triglyceride in the blood are a risk factor for cardiovascular disease and very high levels cause pancreatic inflammation.
- Lipoprotein Little a – LP(a)- A lipoprotein that is genetically inherited in higher levels in 20 percent of the population that multiplies your risk of cardiovascular disease. It should be measured once in your life. Dr. Dinesh comments that this test is underdone and not well known among the medical fraternity but should be done on everyone as it influences how we treat the individual and their future risk.
Lipid panels are useful to monitor and manage hypercholesterolaemia before any serious cardiovascular event takes place. Your doctor may recommend you to get a lipid panel, as well as regular follow-up screenings, if you are a high-risk individual.
How is hypercholesterolaemia treated?
Hypercholesterolaemia treatment requires lifestyle changes and adjustments. Leading a healthy lifestyle is often the first step to managing this condition .
- Dietary changes – Maintaining a healthy diet is important to manage your cholesterol levels, a diet rich in fruits and vegetables, as well as healthy unsaturated fats are generally recommended.
- Increase physical activity – Being more active can improve your overall health and control dyslipidaemia. Exercising for more than 30 minutes a day, 5 times a week is generally recommended to manage cholesterol levels. This should be started gradually. Additionally, incorporating various types of exercises such as resistance training and aerobic exercises is also recommended. Dr. Dinesh has seen many of his patients raise their HDL this way.
- Reduce intake of alcohol and tobacco use – Excessive intake of alcohol and use of tobacco are often associated with an increased risk of cardiovascular diseases. The aim of hypercholesterolaemia management is to reduce strokes and heart attacks.
- Manage stress – Chronic stress can increase cortisol levels in your body, high levels of cortisol is associated with an increase in total cholesterol, HDL-C, and LDL-C in the blood.
- Medications – In cases where lifestyle changes are not enough to control your dyslipidaemia, your doctor may prescribe cholesterol-lowering drugs for you. Common examples of these medications include:
- Statins – Statins are medications that lower your LDL-C by inhibiting 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) activity. This slows down cholesterol synthesis in the liver and increases liver LDL receptors.
- Ezetimibe – Ezetimibe reduces cholesterol absorption in the intestine and increases LDL receptor activity in the liver. Often ezetimibe is used in combination with statins.
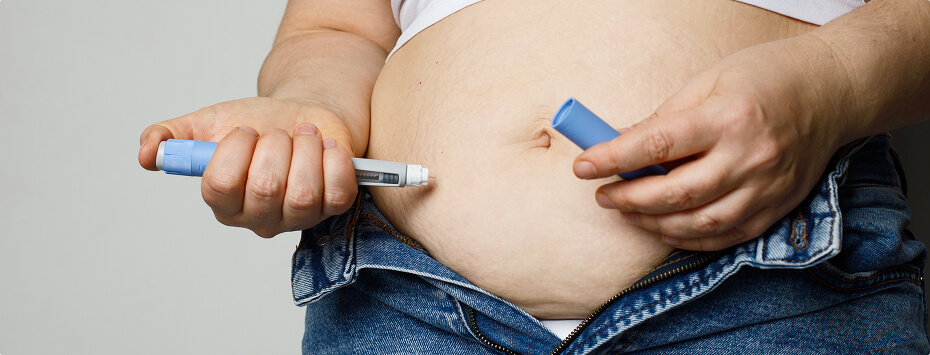
- PCSK9 inhibitors – PCSK9 promotes the degradation of the LDL receptors in the liver, hence inhibiting the activity of this enzyme can improve LDL-C levels in the blood. This medication is typically given in combination with statins to patients at high risk of atherosclerotic cardiovascular diseases.
- Bempedoic acid – Bempedoic acid inhibits the activity of adenosine triphosphate-citrate lyase (ACL), which reduces cholesterol synthesis and increases LDL receptors as well as LDL-C clearance from the blood.
- Omega 3 – Helps reduce triglycerides in those with high triglyceride levels.
What are the complications of hypercholesterolaemia?
Hypercholesterolaemia contributes to the formation of atherosclerotic plaques. These plaques build up in the arterial walls, blocking blood flow. Even more critical is when the blood vessel is suddenly blocked when these plaques rupture and cause blood clots to form. This is what typically happens in a heart attack/ stroke. When left untreated or unmanaged, atherosclerotic plaques can lead to:
- Coronary artery diseases – The coronary artery supplies blood to your heart. An atherosclerotic plaque can block the blood supply to the heart and cause conditions such as shortness of breath, angina, and myocardial infarction (heart attack).
- Carotid artery diseases – The carotid artery supplies blood to your brain, a blockage in this artery can lead to stenosis or strokes.
- Peripheral artery diseases – Plaque build-up in your peripheral arteries can lead to reduced blood flow to your hands and feet. Common symptoms of peripheral artery disease include frequent infections on the limbs and poor wound healing of the limbs.
- Kidney artery stenosis – Kidney artery stenosis refers to the narrowing of the blood vessels that supply blood to your kidneys, this can impair kidney functions and lead to chronic kidney diseases.
- Mesenteric ischaemia – The mesentery is the membrane in the abdomen that holds the bowels. Mesenteric ischaemia caused by atherosclerotic plaques can reduce blood flow to the small intestines, damaging the small intestines.
Summary
Hypercholesterolaemia is a long-term condition caused by a combination of genetic and environmental factors. Thankfully, your cholesterol levels can be effectively managed with regular screening, monitoring, lifestyle changes, and the right medical intervention.
When it comes to lipid disorders, early detection and treatment are essential — left unmanaged, hypercholesterolaemia can lead to serious complications, such as heart disease. Take the first step today and book a consultation with us for a detailed diagnosis and personalised treatment plan.
Frequently Asked Questions
A healthy lifestyle is important to manage and control your cholesterol levels. Maintaining a healthy diet and regular exercise are recommended as it can help lower cholesterol levels and improve your overall health.
Some people may be able to manage their cholesterol levels through diet and exercise alone. In some cases, patients may need to take cholesterol-lowering medications for a long time due to genetic predisposition or a high risk of atherosclerotic cardiovascular diseases. Lifestyle changes reduce cholesterol by 20 percent. Those who need more than that will likely need long-term medication.
You may still eat your usual foods, but it is recommended to reduce the consumption of red meats, processed meats, fatty or greasy foods, and foods with saturated or trans fat. Instead, opt for foods with high fibre, such as fruits and vegetables, whole grains, and healthy fats such as fish and nuts.
It is recommended to visit your doctor for a lipid panel test if you are at risk of hypercholesterolaemia. Individuals aged over 35 for men, and 45 for women are recommended to undergo regular screenings. Additionally, if you have diabetes, a family history of hypercholesterolaemia, obesity, or hypertension, you are also recommended to undergo a lipid panel test.
You will not know if you have high cholesterol until your doctor performs a lipid panel. Hypercholesterolaemia do not typically show symptoms, and the symptoms such as chest pains, difficulty breathing, and dizziness, are typically caused by atherosclerotic plaques in the blood vessels which is too late